Article Links
Timeline
When will this be released?
Release Date: 12/12/2024 from 5:00 – 6:30 pm PDT, PST.
Is there downtime for this release?
No.
Benefits Dashboard Tasks
With this release, the Benefits Dashboard now has a Task section to provide the Administrator with a quick overview of benefit-related incomplete tasks.
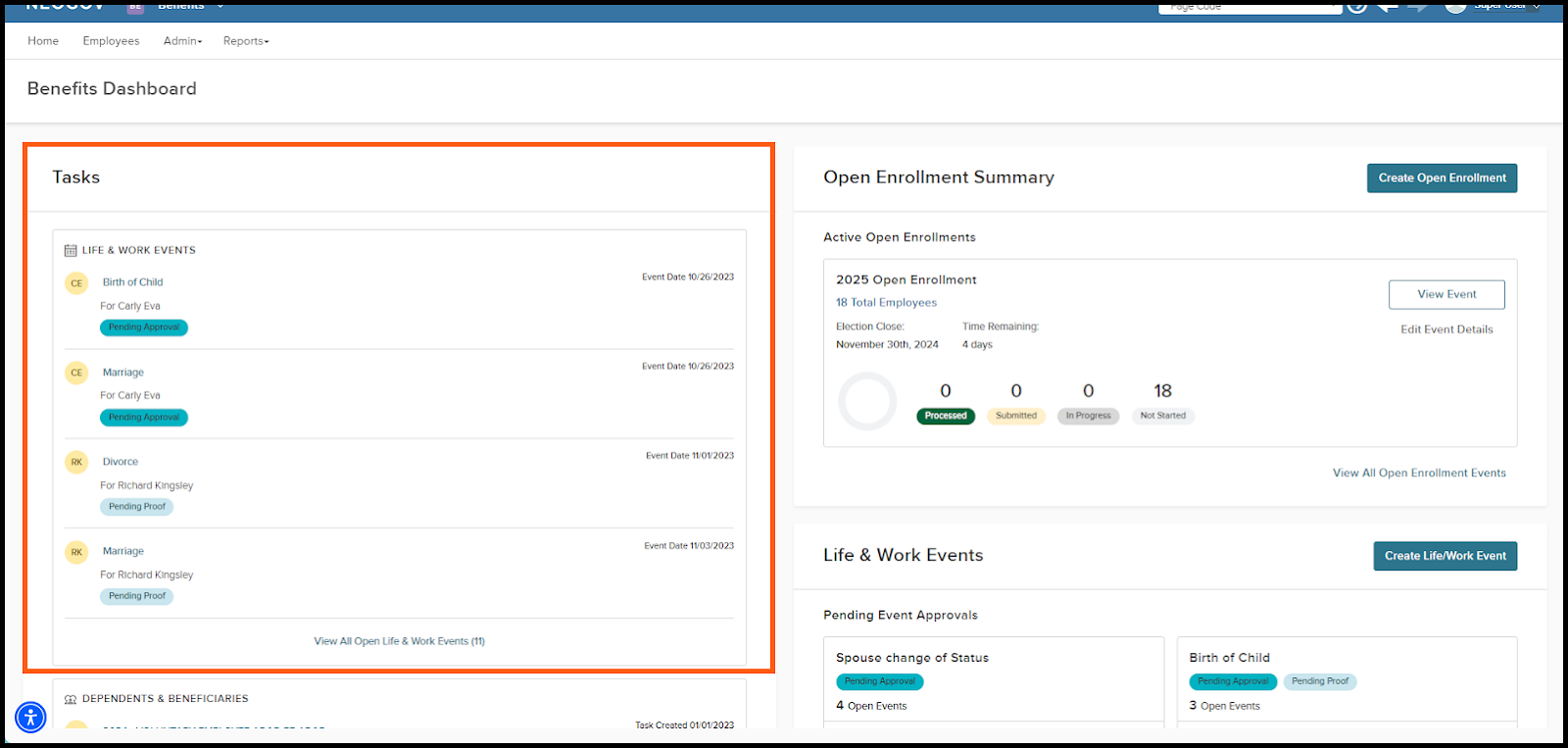
Tasks for Life and Work Events
Each task for Life and Work Events notifies the Administrator of actions, such as Pending Approval and Pending Proof, the agency must collect for an employee's Life/Work Event. Each task has a link directing the Administrator to the Benefit Events page pre-filtered for that specific employee’s Life/Work Event. A link to view all open Life and Work Events will also direct the Administrator to the Benefit Events page pre-filtered to all open Life/Work Events.
Each task will provide the following.
- Life and Work Event Description: This is the link to select to navigate to the Benefit Events page with the table filtered to the specific Life/Work Event for that specific employee.
- For: First Name and Last Name of the Employee.
- Status: Pending Proof or Pending Approval.
- Event Date: The date of the Event.
If no Life and Work Events are Pending Approval or Pending Proof, this task section will not be on the Benefits Dashboard.
When you’ve completed the task and no additional actions are required, NEOGOV removes it from the Life and Work Events task section.
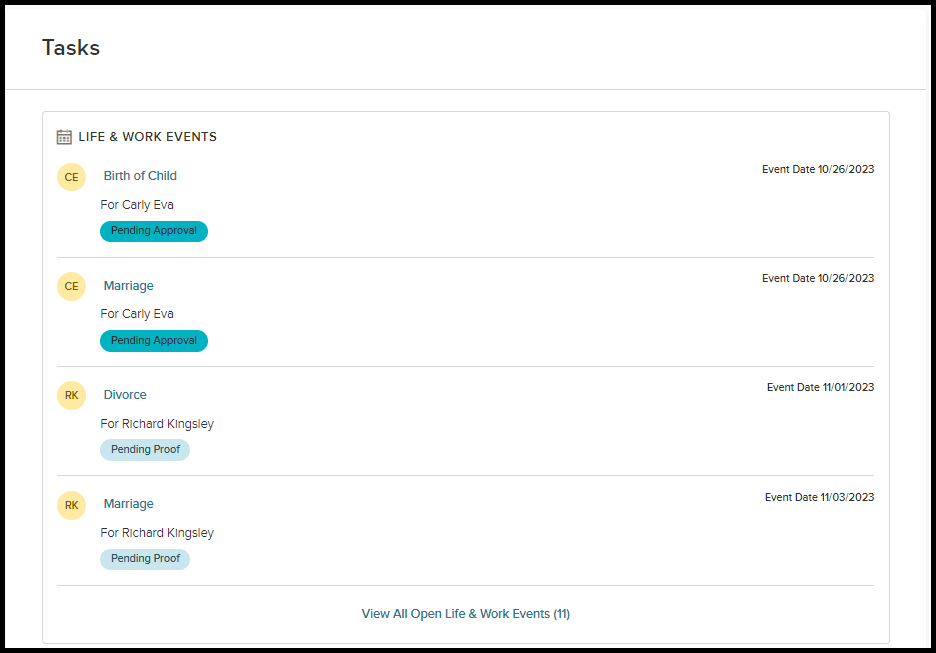
Tasks for Dependents and Beneficiaries
Each task for the Dependents and Beneficiaries notifies the Administrator of the action they must take on an employee’s enrollment. A task will be created for an employee’s enrollment when:
- Aged-out Dependent: Any current or future enrollments have a Dependent aged out (Maximum Child and Maximum Disabled Age).
- Invalid Dependents: Any current or future enrollments have Dependents selected that do not match the recipient type of Coverage.
- Missing Dependents: Any current or future enrollments have the number of Dependents selected that is less than the Minimum Number of Dependents set on the Coverage.
- Excess Dependents: Any current or future enrollments have the number of Dependents selected that exceeds the Maximum Number of Dependents set on the Coverage.
- Missing Beneficiary: Any current or future enrollments have a missing Primary Beneficiary (no Primary Beneficiary selected on the enrollment record).
- Missing Beneficiary %: Any current or future enrollments with missing Primary and Contingent Beneficiary %.
- Invalid Beneficiary %: Any current or future enrollments have Primary and Contingent Beneficiaries that % does not equal 100%.
- Inactive Dependent: Any current or future enrollments have a Dependent attached to an enrollment, but their contact record is inactive.
- Inactive Beneficiary: Any current or future enrollments have a Beneficiary attached to enrollment, but their contact record is inactive.
Each task has a link that will direct the Administrator to the employee’s enrollment to make the necessary corrections.
Each task will provide the following:
- Plan Title and Coverage: The link to select to navigate to the employee’s enrollment.
- For: First Name and Last Name of the Employee.
- Status:
- Aged out Dependent
- Invalid Dependents
- Missing Dependents
- Excess Dependents
- Missing Beneficiary
- Missing Beneficiary %
- Invalid Beneficiary %
- Inactive Dependent
- Inactive Beneficiary
- Task Created On: The task creation date.
If no action is needed on an employee’s enrollment, this task section will not be on the Benefits Dashboard.
When you’ve completed the task and no additional actions are required, NEOGOV removes the task from the Dependents and Beneficiaries task section.
Value
Provide Benefit Administrators with a task list of actions they must take for an employee’s Life and Work Event or on their Enrollments.
Audience
Benefit Administrators.
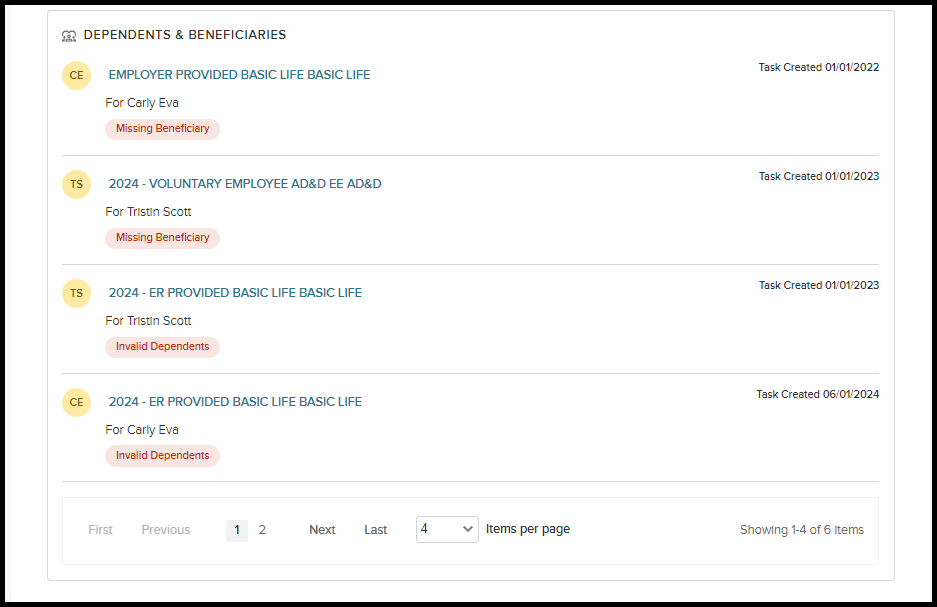
Benefit Plans - Expiration Date
With this release, Administrators can bulk update all current and future enrollments when an Expiration Date is entered or changed on a Benefit Plan.
You can find the Expiration date in the Rules section on the Plan Setup tab of the Benefit Plan. This field determines the enrollment expiration date for all employees enrolled in a plan. We use this date field only when a specific date is required to end enrollment. Otherwise, the expiration date defaults to the employee's termination date. This date is reflected on an employee's enrollment as the Eligibility End Date.
Enter the date in a DD-MON format (for example, 31-DEC). This is the current year, so that 31-DEC would be Dec 31st, 2024.
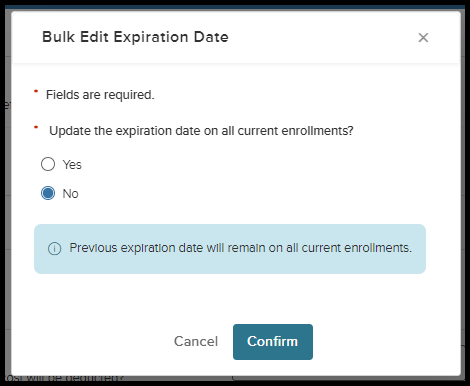
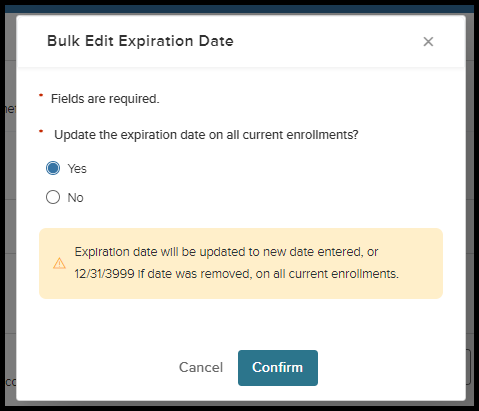
When this date is changed, administrators will be prompted with a question about whether they want to update the expiration date on all current enrollments. If the Administrator selects:
- Yes - then the expiration date will be updated to the new date entered, or 12/31/3999 if the date was removed, on all current enrollments.
- No - then the previous expiration date will remain on all current enrollments (if no expiration date were present before, it would remain 12/31/3999 on all current enrollments.)
When selecting Yes, the process will run in the background, updating all current enrollment records.
Value
Providing Benefit Administrators with the ability to bulk update the expiration date on all current enrollments.
Audience
Benefit Administrators.
Employees - Current Enrollments
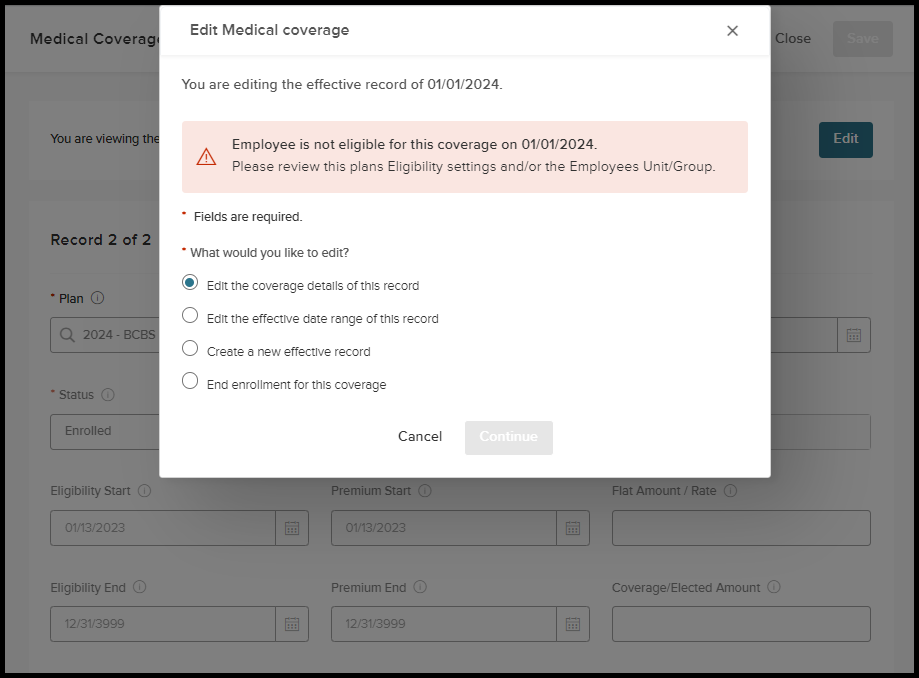
In this release, administrators will receive notifications if an employee enrolled in a plan or coverage is no longer eligible based on the plan's eligibility criteria. When an administrator selects Edit on an employee's current enrollment, it is determined that the employee is no longer eligible as of the current date—considering the Coverage Effective Date and Eligibility requirements—a notice of non-eligibility will appear. Consequently, actions that can be taken regarding enrollment will be restricted.
For example:
An employee was part of an Eligible Unit/Group upon initial enrollment on 01/01/2024. On 11/04/2024, the employee changed their assignment and is no longer in an Eligible Unit/Group for the currently enrolled Plan/Coverage. Upon Edit, an alert will be present notifying the Administrator that the employee is no longer eligible for the Plan/Coverage that was effective on 01/01/2024. The alert advises administrators to review the plan's Eligibility or the employee's Unit/Group. They can take action on the enrollment to:
- Edit the effective date range of this record
- Create a new, effective record
- End enrollment for this coverage
If Administrators believe that it is an error that the employee is no longer eligible for the Plan/Coverage, they would then need to review the Eligibility setup on the Plan or the Unit/Group the Employee is now in.
Value
Providing notifications to Administrators on why they are not able to edit enrollment when it is due to eligibility.
Audience
Benefit Administrators
Appendix: Bugs Resolved
| Scenario | Issue |
| When running payroll with the Benefit Credit Plan, the logic incorrectly retrieves flex amount values from the future Benefit Credit plan rates instead of the current Benefit Credit plan rates. | Payroll with Benefit Credit Plan Type pulls in future rates, causing incorrect payroll calculation. |
| In Open Enrollment, when contact permission is restricted, data from the contact record is unintentionally removed when Save is selected on the pop-up. | In Open Enrollment dependents and beneficiaries, the pop-up removes details upon Save. |

